General Info on ACL
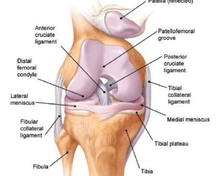
The knee joint is the largest and most complex joint in the human body. In addition to bending and stretching, other movements are also possible in the joint, such as turning and sliding. The natural knee consists of three bones: the thighbone (femur), the shinbone (tibia), and the kneecap (patella). The knee is reinforced with ligaments made up of collagen fibers and embedded in connective tissue called ligaments. On the sides of the knee, the joint is reinforced by the medial and lateral collateral ligament. In addition, there are ligaments that lie in the center of the knee and are called the anterior and posterior cruciate ligament because of their crossed course. An excellent educational video can be found here
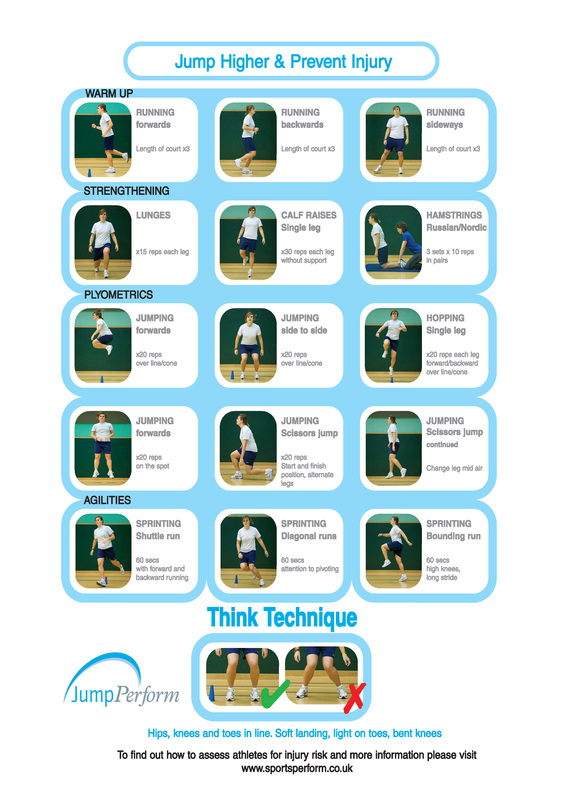
Prevention
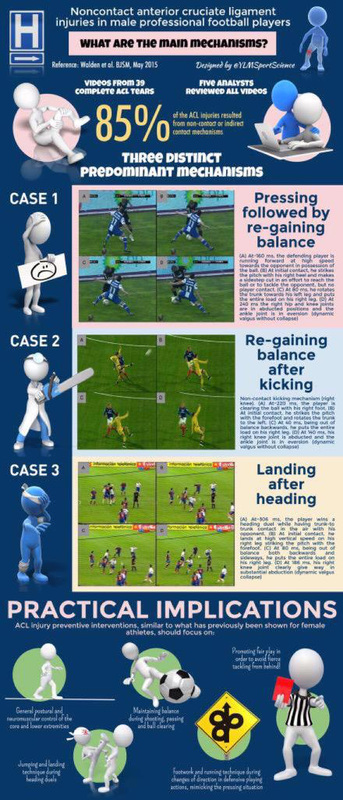
How does an ACL injury occur?
The anterior cruciate ligament mainly functions as a stabilizer of the knee both in anterior-posterior direction and also in rotation. Typical injuries occur during sudden turning maneuvers such as pivot movements or torsions during sports practice. The patient typically reports feeling or hearing a 'crack'. In most cases, at that moment you cannot continue to exercise and the knee swells. Afterwards, one often has a giving way feeling with short rotational movements. Sometimes, however, the symptoms are much more subtle with only mild pain and swelling.
Diagnosis

The diagnosis of a torn anterior cruciate ligament can usually already be made on the basis of the story of 'torsional trauma with a crack'. During the clinical examination, the Lachman, drawer and pivot shift test should be performed. An MRI scanner of the knee is recommended in most cases to detect additional cartilage and meniscus injuries (up to 40%).
Treatment Options
Anterior cruciate ligament injuries can rarely be treated conservatively. Surgery can only be avoided if there are no predominant instability complaints. In most cases, sports with rotational movements should also be avoided. In most patients, on the basis of instability complaints, age, additional meniscus or cartilage injuries, and activity level, a decision will be made to reconstruct the cruciate ligament via surgery. The timing of reconstruction mainly takes into account the stiffness of the knee (should be avoided). The procedure can therefore usually be performed within 6 weeks after the trauma. Ideally, the procedure should be performed before 9 months, since additional stretching of other ligaments often occurs afterwards and the risks of additional meniscal tears increase significantly.
ACL reconstruction
The torn anterior cruciate ligament is replaced with a new cruciate ligament. The hamstring tendons or quadriceps tendon or patellar tendon from your knee can be used for this. The choice of tendon will be discussed with you in advance. In exceptional cases, a donor tendon or artifcial tendon should be used. During the arthroscopy, the old remnants of the damaged cruciate ligament are removed and two tunnels are drilled into the bone: one in the upper leg and one in the lower leg, both ending in the knee at the exact location of your anterior cruciate ligament. The ends of the tunnels in the knee are at the place where the original cruciate ligament attaches to the upper and lower leg. The tendon material is introduced into the knee through the tunnels at the site of the original cruciate ligament (anatomical anterior cruciate ligament reconstruction). The tendon is fixed with a special fixation system. This system is very important, because it must provide firmness until the graft has fully healed and integrated into the bone. In normal circumstances, this is three to six months after the procedure. In selected cases, the anterolateral complex will also be repaired by a MONOLOOP reconstruction. The rest of the knee is also examined and any damage to the cartilage and meniscus repaired. Some meniscal tears can even be stitched.
Anterolateral Instability (ALI)
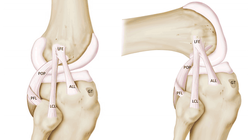
Recent research has shown that anterior cruciate ligament injuries often involve tearing not only of the anterior cruciate ligament, but also of the anterolateral capsule. The anterolateral capsule is an important stabilizer of the pivot movement! The MONOLOOP procedure (performed by our group for over 20 years!) on the outside of the knee repairs this ligament and increases resistance to rotational movements.
ACL repair instead of reconstruction? is it possible?
Recently there has been a lot of scientific interest in repairing the cruciate ligament by means of sutures and an augmentation, instead of the classic reconstruction in which the cruciate ligament is replaced by a tendon graft. In this case, the torn anterior cruciate ligament is not replaced by a tendon, but it is sewn together and reinforced (augmentation). Only 10% of all cruciate ligament tears, ie in which the anterior cruciate ligament ruptures at the femoral origin, could qualify for this. Scientific research is still ongoing to improve this technique because previous research has clearly shown that no good recovery is possible after simple suturing or augmentation. Based on latest scientific data for athletes, we advise against repair and strongly support reconstruction
Revision ACL surgery
Anterior cruciate ligament revision surgery is usually more complex surgery in which, in addition to the anterior cruciate ligament revision, specific attention must also be paid to the position of the former tunnels, the condition of the menisci as well as any additional instability of the medial and lateral ligaments. The different options will be discussed with you, such as tendon graft choices and any need for additional surgery.
Frequently Asked Questions
When can I drive? This depends on the strength and coordination of your knee. Your physiotherapist can assess when participation in traffic is responsible again. Usually this is possible from week 4-6
When can I resume work? This obviously depends on the type of work and can vary from 4 weeks to 4 months
How long should I get the injections for DVT? 20 days
When can I shower? As soon as the wound is dry, a waterproof bandage can be applied so that showering is possible!
Postoperative Problems? in about 5% of cases, full stretching after 3 months of rehabilitation remains difficult. Usually this is due to scar tissue growing around the new ACL. If problematic, this scar tissue can be easily removed via keyhole surgery (usually between months 3 and 6).
How long will I stay in hospital? Classic 1 night
Complications? Blood clotting and phlebitis may occur. If these clots break free, they can travel to the lungs and cause a life-threatening pulmonary embolism. To minimize this risk, injections with a blood thinner are therefore given for 20 days. Infections are rarely seen but can occur either around the wound or deeper around the cruciate ligament. Superficial wound infections can in most cases be treated with antibiotics. Deep infections usually require additional arthroscopic surgery. Antibiotics are given during the procedure to minimize the risk of infection.
When can I resume work? This obviously depends on the type of work and can vary from 4 weeks to 4 months
How long should I get the injections for DVT? 20 days
When can I shower? As soon as the wound is dry, a waterproof bandage can be applied so that showering is possible!
Postoperative Problems? in about 5% of cases, full stretching after 3 months of rehabilitation remains difficult. Usually this is due to scar tissue growing around the new ACL. If problematic, this scar tissue can be easily removed via keyhole surgery (usually between months 3 and 6).
How long will I stay in hospital? Classic 1 night
Complications? Blood clotting and phlebitis may occur. If these clots break free, they can travel to the lungs and cause a life-threatening pulmonary embolism. To minimize this risk, injections with a blood thinner are therefore given for 20 days. Infections are rarely seen but can occur either around the wound or deeper around the cruciate ligament. Superficial wound infections can in most cases be treated with antibiotics. Deep infections usually require additional arthroscopic surgery. Antibiotics are given during the procedure to minimize the risk of infection.