What causes cartilage lesions?
Due to trauma (accident), microtrauma (overload) or degeneration (age and wear). The pain in such an injury is caused by the defect in the cartilage and excess pressure on the underlying bone, causing bone marrow swelling and pain. The associated swelling can also cause pain in the joint.
Can we treat all cartilage lesions?
Trauma and micro-traumatic injuries are quite treatable, but this is more difficult for degenerative injuries. Patients over the age of 50 are less eligible for a biological option. If cartilage injuries are not treated, the layer of cartilage can gradually wear away, resulting in osteoarthritis and progressive immobility.
Treatment options
Currently there are various therapies depending on age, severity and level of activity. Medication: Classic pain relief (paracetamol and anti-inflammatory drugs) and glucosamine preparations are often used in the first phase of treatment or after surgery. Weight reduction: by reducing the load on the knee joint, the pain will decrease significantly. If you are seriously overweight (BMI over 35), an appointment is usually proposed at the obesity clinic. Adapted Activities and Physiotherapy: Cycling, swimming and low impact activities such as fitness are excellent for the knee joint.
Injections with cortisone, hyaluronic acid, plateletrich plasma (PRP) and microfragmented fat
Osteoarthritis or wear and tear of cartilage and meniscus tissue is a frequent problem. The onset of osteoarthritis is a complex phenomenon and is still not fully understood. What we do know is that several causes are at the root of this condition. For example, we know that people with sports injuries such as a tear of the cruciate ligament or meniscus have a strongly increased risk of osteoarthritis 20-25 years after the trauma because the cartilage is exposed to increased shear and compressive forces. Osteoarthritis can also be accelerated by an abnormality in the shape of the knee, such as with O- or X-leg, trochleodysplasia and condylar abnormalities, eg a small medial or lateral femoral condyle. We also know that osteoarthritis occurs more often in certain families due to genetic abnormalities. Of course, the knee will also wear out more if you use it too intensely, or if you are overweight… The treatment of osteoarthritis therefore consists on the one hand of making the knee as strong as possible, and on the other hand of reducing certain risk factors. However, healing is impossible.
Strengthening physiotherapy and supportive measures such as weight reduction and simple pain medication can already make a big difference!
An injection of cortisone can quickly suppress the inflammation and inflammation present in a damaged joint and reduce pain. However, frequent (more than 2 per year) injections of cortisone are not recommended because cortisone use can also have adverse effects on healthy tissues. That is why we still recommend 1 to 2 injections of cortisone in swollen and painful joints. If the pain and swelling persist, additional measures must often be taken.
Hyaluronic acid is a natural lubricant in the knee and has a nourishing and protective effect on the cartilage. Recent data show that an injection of 1 high dose of hyaluronic acid is equivalent to the injections of several small injections. Hyaluronic acid is often also combined with an anti-oxidant.
Platelets are cells in the blood that are rich in growth factors that are normally released when damaged to speed up healing and attract stem cells. These platelets can be concentrated by a simple blood draw and then injected into the knee. Usually 3 injections are needed to initiate a proper healing response.
Fat and stem cell injections have been getting a lot of attention lately and are seen by some specialists as the 'holy grale' to treat osteoarthritis. However, there is not much scientific data yet. We do know for sure that these stem cells are present around blood vessels, in bone marrow and in adipose tissue. Their number decreases with age. These stem cells are abundant in abdominal fat and can be harvested and activated there under local anesthesia. They are then injected back in their natural fat-rich solution into the knee (or another joint) to suppress local inflammation and help repair the lesions. More information can be found here. All the injections mentioned can therefore help to make a worn-out joint stronger and less painful. Each type of injection has its advantages and disadvantages. However, there is no refund for injections except with cortisone! Most frequent side effect for all injections is pain and swelling in response to the injection.
Strengthening physiotherapy and supportive measures such as weight reduction and simple pain medication can already make a big difference!
An injection of cortisone can quickly suppress the inflammation and inflammation present in a damaged joint and reduce pain. However, frequent (more than 2 per year) injections of cortisone are not recommended because cortisone use can also have adverse effects on healthy tissues. That is why we still recommend 1 to 2 injections of cortisone in swollen and painful joints. If the pain and swelling persist, additional measures must often be taken.
Hyaluronic acid is a natural lubricant in the knee and has a nourishing and protective effect on the cartilage. Recent data show that an injection of 1 high dose of hyaluronic acid is equivalent to the injections of several small injections. Hyaluronic acid is often also combined with an anti-oxidant.
Platelets are cells in the blood that are rich in growth factors that are normally released when damaged to speed up healing and attract stem cells. These platelets can be concentrated by a simple blood draw and then injected into the knee. Usually 3 injections are needed to initiate a proper healing response.
Fat and stem cell injections have been getting a lot of attention lately and are seen by some specialists as the 'holy grale' to treat osteoarthritis. However, there is not much scientific data yet. We do know for sure that these stem cells are present around blood vessels, in bone marrow and in adipose tissue. Their number decreases with age. These stem cells are abundant in abdominal fat and can be harvested and activated there under local anesthesia. They are then injected back in their natural fat-rich solution into the knee (or another joint) to suppress local inflammation and help repair the lesions. More information can be found here. All the injections mentioned can therefore help to make a worn-out joint stronger and less painful. Each type of injection has its advantages and disadvantages. However, there is no refund for injections except with cortisone! Most frequent side effect for all injections is pain and swelling in response to the injection.
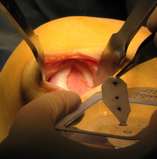
Shaving en Debridement
During keyhole surgery, the loose cartilage pieces are removed using a shaver. The edges of the cartilage injury are stabilized.
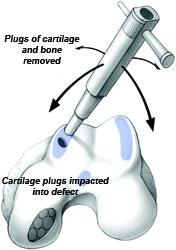
Microfracture or Ice-picking

Microfracture or ice-picking: during exploratory surgery, small holes are made in the underlying bone with an ice-pick. When ice-picking, the bone marrow bubbles through the holes in the injury, allowing a blood clot with stem cells to fill the cartilage injury. These stem cells can then produce repair tissue. This technique is suitable for isolated cartilage injuries up to 1.5 square cm. A recent study has shown that adding certain gels and scaffolds can optimize healing after microfracture. These techniques are called Microfracture +
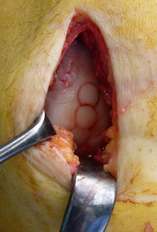
Autologous chondrocyte transplantation
In a first step, pieces of cartilage are removed during keyhole surgery (biopsy). These cartilage pieces are sent to the lab where the cells are cultured for about 10 weeks. In a second step, these cells are then implanted during an open procedure through a mini-incision. The cells are first seeded onto a collagen membrane that is sutured or adhered into the lesion. This technique is suitable for isolated cartilage lesions of 2-10 square cm. Unfortunately, this technique is no longer available in Belgium and Europe since June 2016!
Cartilage Scaffolds

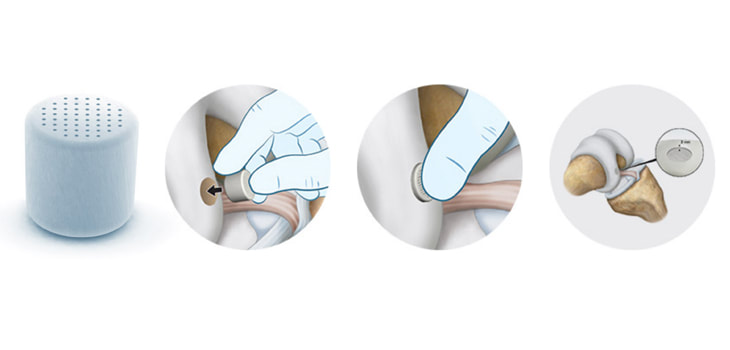
For injuries in which both cartilage and bone are affected, an artificial cartilage membrane or scaffold can be implanted. This scaffold allows to restore both bone and cartilage through 1 operation. Scaffolds come in the form of plugs or foam.
Metal Implants

In case of focal lesions of the cartilage and subchondral bone, complex cartilaginous lesions or in slightly older patients, a non-biological solution can be opted for. The cartilage damage is covered with a metal implant that can be custom-made for the patient. This patient-specific technology is a powerful and robust solution and is well researched
Rehabilitation
Rehabilitation also plays a very important role in recovery and starts the day after surgery. With regard to rehabilitation, it is important to be well informed and guided. A full rehabilitation period can take up to a year. Sport is slowed down during the first year and up to 18 months after the procedure. Other precautions include wearing a brace for three months and an initial brace ban for two to four weeks.