Anatomy of the healthy knee

The knee joint is the largest and most complex joint in the human body. In addition to bending and stretching, other movements are possible in the joint, such as turning and sliding.
The natural knee consists of three bones: the thighbone (femur), the shinbone (tibia), and the kneecap (patella). In the knee joint, the ends of the femur, tibia, and back of the kneecap are covered with smooth cartilage. This cartilage allows smooth movement between the two bone ends. When a healthy knee makes a movement, the two articular surfaces move easily and without pain relative to each other. Between the two ends of the femur and tibia is another cartilaginous structure called the "meniscus," which acts as a damper. The knee joint is closed by a joint capsule, which contains a membrane. Strong ligaments connect the femur to the tibia, covering the joint and stabilizing it. The movements of the knee are directed and controlled by the strong thigh muscles (quadriceps) and the muscles of the lower leg. A healthy knee allows the leg to move freely within its range of motion and absorbs the shock created by activities such as walking and running.
The natural knee consists of three bones: the thighbone (femur), the shinbone (tibia), and the kneecap (patella). In the knee joint, the ends of the femur, tibia, and back of the kneecap are covered with smooth cartilage. This cartilage allows smooth movement between the two bone ends. When a healthy knee makes a movement, the two articular surfaces move easily and without pain relative to each other. Between the two ends of the femur and tibia is another cartilaginous structure called the "meniscus," which acts as a damper. The knee joint is closed by a joint capsule, which contains a membrane. Strong ligaments connect the femur to the tibia, covering the joint and stabilizing it. The movements of the knee are directed and controlled by the strong thigh muscles (quadriceps) and the muscles of the lower leg. A healthy knee allows the leg to move freely within its range of motion and absorbs the shock created by activities such as walking and running.
The degenerative knee
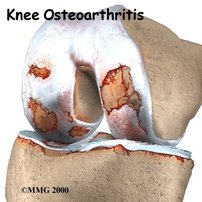
Knee wear is characterized by wear and tear of the cartilage and meniscus. Small cracks, pits and tears appear in these tissues. As a result, you will experience pain, swelling and function less well (walking, climbing stairs, cycling). Wear and tear usually occurs due to age, but can also occur at a younger age due to rheumatism or as a result of an accident. Wear and tear is more often seen in people with heavy work, a long time after a sports accident and in overweight people.
Knee Arthroplasty Algemeen
The purpose of implanting a knee replacement is:
- Reducing pain and improving quality of life.
- Correct any deformities, for example o-legs or x-legs.
- Restore any loss of function in your knee.
Total Knee Arthroplasty

The ends of the femur and tibia are provided with a new surface. The kneecap does not always get a new layer.
Each knee prosthesis consists of several parts
1. The femoral (thigh bone) portion forms the new surface of the femur and is made of a metal alloy.
2. Although the kneecap doesn't always get a new layer, the kneecap portion replaces the bottom of the kneecap and rubs against the thigh bone. The kneecap part is completely made of plastic.
3. The lower leg section is two-piece.
The two-part variant consists of a metal surface that is attached to the bone and a plastic insert (polyethylene or PE) for a smooth surface over which the thigh bone slides.
Each knee prosthesis consists of several parts
1. The femoral (thigh bone) portion forms the new surface of the femur and is made of a metal alloy.
2. Although the kneecap doesn't always get a new layer, the kneecap portion replaces the bottom of the kneecap and rubs against the thigh bone. The kneecap part is completely made of plastic.
3. The lower leg section is two-piece.
The two-part variant consists of a metal surface that is attached to the bone and a plastic insert (polyethylene or PE) for a smooth surface over which the thigh bone slides.
3D gepersonaliseerde prothese
Since June 2021, a custom-made 'personalized' prostheses is available on the Belgian market. This prosthesis has the advantage that the anatomy of the patient can be fully respected, with theoretically fewer compromises in terms of size, contour and joint line of the prosthesis. Slight to moderate axial deviations can be handled smoothly. Serious abnormalities cannot yet be treated.
Unicompartimental Knee Arthroplasty (UKA)

Only one part of the knee is damaged and only this part gets a new surface. The parts of the knee that are not damaged do not get a new layer.
Patello-Femoral Arthroplasty
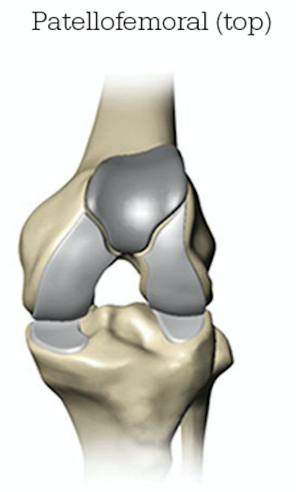
Only the kneecap and the trochlea (another word for the gutter in which the kneecap runs) are replaced. The parts of the knee that are not damaged are not replaced.
Revision Total Knee Arthroplasty

Re-surgery of a previously placed knee prosthesis that has worn out, is not working properly, or has become loose.
The previously placed parts are removed in whole or in part and replaced by new ones. Usually the revision prosthesis is larger and extended by means of a stem for better fixation.
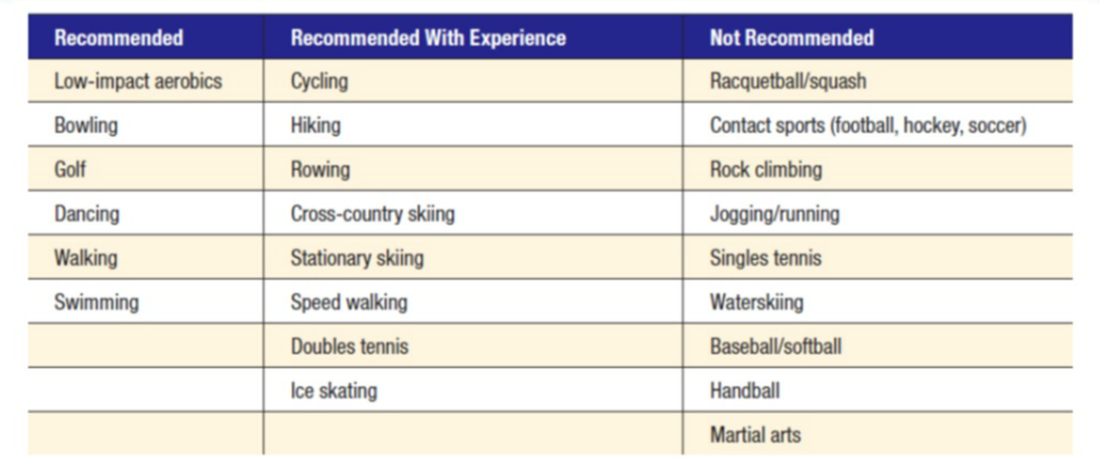
Allowed Activities (according to American Knee Society)
Antwerp Advanced Anesthesia (3A)
Multimodal anesthesia and pain management are essential for successful prosthetic surgery. In recent years there has been a huge evolution and improvement in this specialization, enabling faster rehabilitation, better pain control and a smooth return home. For knee prosthesis surgery, a combination of epidural with light sedation, local injection anesthesia (LIA) around the joint and dexamethasone are usually used as postoperative pain relief (better known as Antwerp Advance Anesthesia or 3A); or general anesthesia with femoral block and LIA. With full anesthesia, the whole body is numb and you are unconscious for a while. With 3A, the body below the bellybutton is completely numb, while the rest of the body continues to function normally. Because there is less pain, the use of strong painkillers (such as morphine) can be reduced, so that fewer side effects occur. Most patients with 3A can walk out of bed the same day and mobilize faster. Feel free to talk to your anesthetist about it!
Frequently Asked Questions
At what age is a prosthesis placed? Most prostheses are placed between the ages of 57 and 77 with an average of 67.5 years, 2/3 of which are female patients.
What are the complaints BEFORE the operation? Typically, patients will report being able to walk for less than 1 hour and having daily pain with frequent use of analgesics before a prosthesis is placed. The RX should show a clear narrowing of the joint space. In exceptional cases, a prosthesis may prove necessary at a younger age (less than 55 years), but more complications are also seen in these younger patients. Alternative treatments such as pain relief, injections, physiotherapy, staying active and weight reduction should be tried before proceeding with the placement of a prosthesis. Talk to your doctor about it!
When can I drive? This depends on the strength and coordination of your knee. Your physiotherapist can assess when participation in traffic is responsible again. Usually this is possible from week 4-6
When can I resume work? This obviously depends on the type of work and can vary from 6 weeks to 6 months
How long should I get the injections for DVT? 40 days
When can I shower? As soon as the wound is dry, a waterproof bandage can be applied so that showering is possible!
How long will I stay in hospital? Our target is 3 nights. As soon as the wound is dry and the physiotherapy is going smoothly, you can go home!
Is it normal for the skin on the outside of the knee to feel numb right next to the scar? This is indeed normal and is explained by the fact that the cutaneous nerves run from the inside of the knee to the outside. When the skin is incised, a few skin nerves will therefore be cut through, causing a numbness in this zone just beyond the scar, on the outside of the knee. This zone can be quite large in the beginning and often shrinks during the first year, but it never disappears.
Complications? Complications after total knee replacement surgery are rare. Serious complications such as infections occur in less than 2% of cases. Major complications such as a heart attack or stroke are even rarer. More complications can be noted in chronic conditions. Although rare, complications can complicate or limit rehabilitation. Discuss this at length with your doctor before surgery Blood clotting and phlebitis may occur. If these clots break free, they can travel to the lungs and cause a life-threatening pulmonary embolism. To minimize this risk, therefore, injections with a blood thinner are given for 40 days. Infections can occur around the wound or deeper around the prosthesis. This can occur immediately after the placement of the prosthesis, during your hospital stay or even much later. Superficial wound infections can in most cases be treated with antibiotics. Deep infections usually require additional surgery, which may even require removal of the prosthesis. Any infection e.g. tooth abscess or urinary tract infection can spread to the denture. Antibiotics are given during the procedure to minimize the risk of infection.
The design and materials from which prostheses are made are undergoing steady improvements. Nevertheless, prosthetic components can wear out and become loose. Although an average bend of 120 degrees is achieved, excessive scar tissue can form and stiffen the joint. This is more often noted in younger patients and patients with limited mobility before surgery. A limited number of patients will still have pain after surgery. Damage to blood vessels and nerves is extremely rare but can happen during surgery.
What are the complaints BEFORE the operation? Typically, patients will report being able to walk for less than 1 hour and having daily pain with frequent use of analgesics before a prosthesis is placed. The RX should show a clear narrowing of the joint space. In exceptional cases, a prosthesis may prove necessary at a younger age (less than 55 years), but more complications are also seen in these younger patients. Alternative treatments such as pain relief, injections, physiotherapy, staying active and weight reduction should be tried before proceeding with the placement of a prosthesis. Talk to your doctor about it!
When can I drive? This depends on the strength and coordination of your knee. Your physiotherapist can assess when participation in traffic is responsible again. Usually this is possible from week 4-6
When can I resume work? This obviously depends on the type of work and can vary from 6 weeks to 6 months
How long should I get the injections for DVT? 40 days
When can I shower? As soon as the wound is dry, a waterproof bandage can be applied so that showering is possible!
How long will I stay in hospital? Our target is 3 nights. As soon as the wound is dry and the physiotherapy is going smoothly, you can go home!
Is it normal for the skin on the outside of the knee to feel numb right next to the scar? This is indeed normal and is explained by the fact that the cutaneous nerves run from the inside of the knee to the outside. When the skin is incised, a few skin nerves will therefore be cut through, causing a numbness in this zone just beyond the scar, on the outside of the knee. This zone can be quite large in the beginning and often shrinks during the first year, but it never disappears.
Complications? Complications after total knee replacement surgery are rare. Serious complications such as infections occur in less than 2% of cases. Major complications such as a heart attack or stroke are even rarer. More complications can be noted in chronic conditions. Although rare, complications can complicate or limit rehabilitation. Discuss this at length with your doctor before surgery Blood clotting and phlebitis may occur. If these clots break free, they can travel to the lungs and cause a life-threatening pulmonary embolism. To minimize this risk, therefore, injections with a blood thinner are given for 40 days. Infections can occur around the wound or deeper around the prosthesis. This can occur immediately after the placement of the prosthesis, during your hospital stay or even much later. Superficial wound infections can in most cases be treated with antibiotics. Deep infections usually require additional surgery, which may even require removal of the prosthesis. Any infection e.g. tooth abscess or urinary tract infection can spread to the denture. Antibiotics are given during the procedure to minimize the risk of infection.
The design and materials from which prostheses are made are undergoing steady improvements. Nevertheless, prosthetic components can wear out and become loose. Although an average bend of 120 degrees is achieved, excessive scar tissue can form and stiffen the joint. This is more often noted in younger patients and patients with limited mobility before surgery. A limited number of patients will still have pain after surgery. Damage to blood vessels and nerves is extremely rare but can happen during surgery.