Introduction

The patellofemoral joint (= the joint between kneecap and femur) is a complex joint in which stability problems (part 1), cartilage injuries and osteoarthritis pain problems (part 2), pain problems (part 3) often occur. These problems should be properly separated from each other as they each deserve a different approach.
It is important to know that the kneecap has to undergo up to 8 times the body weight when climbing stairs, descending, jumping and landing. Also in deep flexion or squatting, an enormous amount of force passes through this joint. Hence the frequent problems.
Part 1
Patella dislocation and instability
Patellar dislocation and instability usually first appear in young people between the ages of 14 and 24 years. The underlying reason is an abnormality in the shape of the femur and patellar shape in which the trochlea (trough of the femur into which the kneecap should slide) is flattened (trochleodysplasia). This allows the kneecap to dislocate laterally or dislocate more easily. In certain cases, the position of the kneecap is too high (patella alta), the attachment point of the patellar tendon on the tibia is too lateral (increased TAGT distance), and/or the kneecap is tilted too much (patellar tilt). The more serious these abnormalities are in the knee, the earlier the first dislocation will often occur. Exceptionally, a dislocation can occur in someone without risk factors during sports where a direct blow is given to the kneecap. During a patellar dislocation, the Medial PatelloFemoral Ligament (MPFL) always tears, which naturally increases the risk of a second patellar dislocation. In recent years, therefore, the surgical approach of patellar dislocations has focused on reconstruction of the MPFL ligament with excellent results. In some patients, a cartilage injury can occur during a dislocation. However, most of these injuries do not require treatment as restoration of stability by MPFL reconstruction often spontaneously accomplishes healing of the cartilage injury.
MPFL Reconstruction
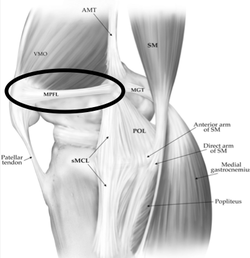
A autologous tendon (gracilis or semitendinosus) is usually used for reconstruction of the MPFL ligament. This tendon is attached to the femur and the kneecap, preventing the kneecap from luxating outwards. Because this reconstruction is 4 times as strong as the original ligament, the stability of the kneecap will be sufficiently restored in the majority of patients.
Concommitant surgery
In some cases, the kneecap is too high (patella alta) and insufficient effect can be obtained with MPFL reconstruction alone. In that case, the position of the kneecap should be lowered by means of a tibial tuberosity transfer. In other cases, the point of attachment of the kneecap to the tibia is too lateral and thus needs to be medialised. In some cases, the trochleodysplasia is very severe and a trochleoplasty should be performed. The indications for additional surgery should be considered on a case-by-case basis by your surgeon.
Part 2
Cartilage lesions and osteoarthritis
Cartilage injuries at the level of the kneecap and trochlea originate either infrequently from obvious trauma (eg fall on the knee or patellar luxation) or frequently from microtrauma. These microtraumas are often accumulations of small injuries due to minimal but long-term overload, eventually resulting in cartilage injuries. This is also the explanation that most cartilage injuries are seen at a somewhat older age between 35-45 years. However, most patients come when the entire cartilage is worn out and the knee therefore shows osteoarthritis. Treatment of cartilage lesions in old age is usually conservative by means of physiotherapy, Injections with hyaluronic acid or cortisone. In specific cases there may be a surgical indication for arthroscopy, cartilage treatment or moving/relieving the kneecap (Fulkerson Procedure). In case of osteoarthritis, prosthesis surgery may be necessary. Typically, these patients are slightly younger (50-60 years) than the classic prosthesis patient (65+).
Part 3
Anterior Knee Pain
Anterior Knee Pain or pain in the front of the knee joint is common. This problem often seen in young girls and ladies (12-25 years). There is no story of obvious instability nor are there any obvious abnormalities visible on the imaging. These patients should be treated conservatively through information, specific physiotherapy and possibly nutritional supplements. There is no surgical indication here. Although often long-term in nature, most complaints disappear spontaneously after the age of 25 years...

